As you enter the healthcare field as a provider, you immediately encounter paperwork, credentialing processes, and compliance requirements. One name that frequently appears is CAQH—the Council for Affordable Quality Healthcare.
CAQH offers an easy way for providers to share their professional and practice details securely with health plans and insurance companies. Instead of filling out the same forms repeatedly for every payer, you enter your information once through CAQH, and insurers can access it whenever they need to verify your credentials.
CAQH credentialing focuses on making the enrollment process faster, easier, and more accurate for both payers and providers. It saves time, reduces paperwork, and helps prevent delays in getting approved to see patients and receive payments. Hospitals, health plans, and other organizations use the CAQH system to maintain current provider data and ensure it complies with industry standards.
Whether you are new to private practice or expanding your services, understanding how CAQH works is crucial to staying connected with payers and keeping your practice running smoothly. Moreover, if you’ve ever wondered how to streamline the credentialing process or why all insurers seem to request the same information, CAQH is the system behind it. Its centralized database allows you to collect and share your professional and practice information efficiently with health insurance organizations.
In this guide, I will break down what CAQH credentialing is, why it matters for your practice, and how you can leverage it to your advantage.
What is CAQH?
CAQH, or the Council for Affordable Quality Healthcare, is a non-profit organization dedicated to streamlining the business side of healthcare. One of its most widely used technologies is CAQH ProView—a centralized database that stores the provider information required for credentialing.
Through this platform (formerly known as the CAQH Provider Data Portal), medical professionals can efficiently manage and share their practice and professional data with multiple health plans and healthcare organizations.
Purpose of CAQH Credentialing
Essentially, the primary goal of CAQH credentialing is to streamline and standardize how healthcare practitioners submit their professional information to payers. It provides a centralized platform where providers can enter and update their credentialing data, which is then shared with participating health plans and other organizations.
Instead of sending credentials to each company individually, providers enter their information once into CAQH ProView, a secure online portal. From there, they can authorize specific health plans and organizations to access their data.
By centralizing the credentialing process, CAQH significantly reduces the administrative burden and associated costs for both providers and payers.
This system ensures that insurance companies have current and accurate providers’ information, which is essential for:
- Verifying providers qualification
- Establishing a network and participation
- Processing claims efficiently
- Maintaining compliance with industry regulations
How CAQH Credentialing Works
Credentialing through the Council for Affordable Quality Healthcare (CAQH) is a vital step for healthcare practitioners who want to join insurance networks and provide care through health plans. The CAQH ProView platform simplifies this process by allowing providers to securely submit, update, and share their professional and practice information with multiple health plans and organizations.
Understanding how CAQH credentialing works can help providers save time, reduce administrative workload, and stay compliant with payer requirements.
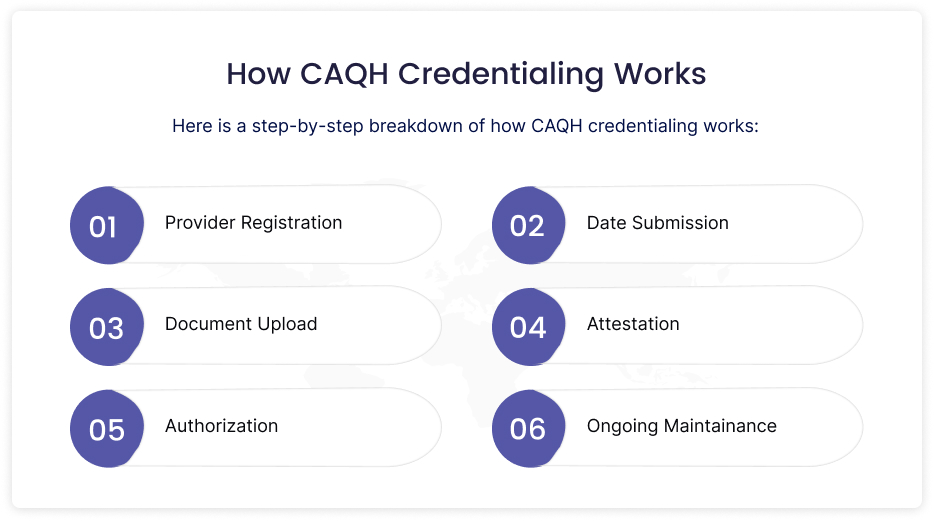
Provider Registration
A healthcare provider creates a profile in CAQH ProView either after receiving an invitation from a participating health plan or by initiating the process on their own.
Date Submission
The provider enters detailed personal, professional, and credentialing information into the CAQH system, including licensure, education, work history, malpractice insurance details, and certifications.
Document Upload
Providers upload supporting documents such as copies of licenses, DEA certificates, liability insurance, and board certifications.
Attestation
Once all the data is entered, the provider must electronically attest that the information is accurate. Providers are required to re-attest to CAQH every 120 days.
Authorization
The provider allows health plans to view their profile. The data can only be viewed by authorized organizations.
Ongoing Maintainance
To keep their information up to date, providers must re-attest regularly and update their CAQH profile whenever changes occur.
Benefits of CAQH Credentialing
Healthcare organizations and providers benefit greatly from CAQH credentialing because it streamlines and speeds up what is often a complex process. By centralizing the collection and management of provider information, CAQH improves accuracy, minimizes repetitive data entry, and reduces paperwork. Consequently, this streamlined approach not only saves valuable time but also helps providers get credentialed faster, allowing them to focus more on patient care and less on administrative tasks.
For Providers
- Saves Time: Instead of submitting their information to multiple organizations repeatedly, providers enter it just once.
- Reduces Paperwork: The digital platform reduces the need for faxing or mailing physical documentation.
Improves Accuracy: Centralized data reduces errors and duplication. - Speeds Up Enrollment: Faster credentialing accelerates provider enrollment and participation in insurance networks.
For Payers and Organizations
- Streamlines Credentialing: Health plans can quickly access and verify provider information.
- Ensures Compliance: Updated data helps meet regulatory and accreditation standards.
- Reduces Administrative Costs: Automation helps reduce the costs associated with data collection and management.
Who Uses CAQH Credentialing?
An extensive variety of stakeholders in the healthcare system use CAQH credentialing:
- Health Insurance Companies (Payers): Well-known commercial carriers like Aetna, Cigna, UnitedHealthcare, Blue Cross Blue Shield, and Humana.
- Hospitals and Health Systems: Many healthcare facilities use CAQH profiles for medical staff credentialing and onboarding.
- Third-Party Credentialing Services: These services often manage provider credentialing on behalf of organizations using CAQH data.
The Role of CAQH in Provider Enrollment
Credentialing is a crucial part of the provider enrollment process. Therefore, the payer must verify the provider’s credentialing before the provider can bill the insurance company or join its network. CAQH streamlines this by serving as a single source of verified information.
Here is how CAQH fits into provider enrollment:
- Providers complete their CAQH profile.
- To access authorized provider information, health plans retrieve data directly from CAQH.
- Once accepted, providers join the health plan’s network and can begin treating patients.
By using CAQH to reduce onboarding delays for both payers and providers, healthcare professionals can begin delivering care sooner and receive payment faster.
Conclusion
What exactly is CAQH credentialing? CAQH credentialing refers to the process that allows healthcare providers to securely share their credentials with insurance companies and healthcare organizations through a centralized, digital platform. It also streamlines the solution by speeding up the enrollment process, reducing paperwork, and improving overall efficiency. Therefore, understanding and utilizing CAQH credentialing is crucial for maintaining a compliant and efficient practice, whether you are a medical administrator, an independent practitioner, or part of a large healthcare system.
Need Help with CAQH Credentialing or Provider Enrollment?
Consider working with Kansas Medical Billing. We have a team of credentialing specialists to ensure accuracy, timeliness, and compliance.